Page Content
Contrary to popular belief, it is not just a teenage disease. When you count 6 million people suffering from this disease, you’ll notice that 30% are women between the ages of 25 and 40 years.
Acne does not manifest itself in the same way in all individuals. There are several different types, with varying degrees of severity.
However, regardless of the type of acne, one of the basic elements is a hypersecretion of sebum. This is called hyperseborrhea and promotes inflammation of the pilosebaceous follicle.
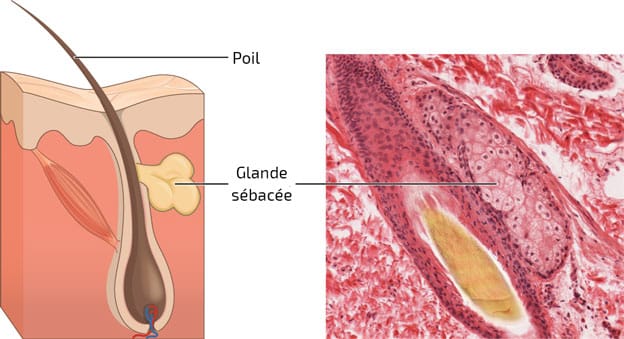
What is a pilosebaceous follicle?
It is the association of a sebaceous gland with a hair follicle (hair). There are several forms.
Sebaceous gland
Definition
A sebaceous gland is an anatomical unit responsible for the secretion of sebum. Generally, its size is inversely proportional to the size of the corresponding hair.
This exocrine gland releases its secretion product in the infundibulum. It is located in the middle part of the dermis, in contact with the pilosebaceous follicle. It is found everywhere on the body, except in the lower lip, the soles of the feet and the palms of the hands.
The density of sebaceous glands depends on the area of the body, but overall, the human species has about 2 million sebaceous glands for every 6 million hairs.
Structure
Sebaceous glands are made up of many cell bases.
Three cell types can be distinguished:
- Basal cells
- Differentiated cells (basal cells loaded with lipids)
- Two kinds of undifferentiated cells; some within the lobules in the irregular septa and others near the basement membrane.
Also found near the latter kind are melanocytes and Langerhans cells.
The sebaceous duct as well as its lower part (the infra-infundibulum) consists of a keratinizing epithelium that is characterized by an absence of granular layer.
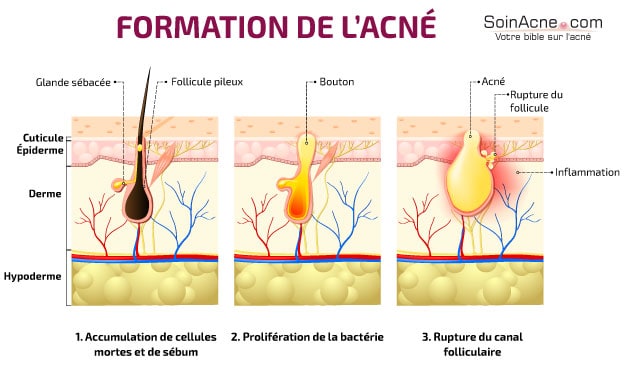
In the absence of acne, the desquamating cells of the infra-infundibulum are easily eliminated through the pilosebaceous orifice, along with the sebum: this is possible because these cells are not very adherent.
In acne, the keratinized cells clump together to form a microcomedo, which prevents the flow of sebum.
Follicle shapes
The pilosebaceous follicle is the combination of the sebaceous gland and the hair.
It can be distinguished in three forms: the sebaceous follicle, the downy follicle and the terminal follicle.
The sebaceous follicle is unique to the human species: it is not present in any other animal species. It is formed by a large, multilobular sebaceous gland. This gland leads to the infundibulum via numerous sebaceous ducts.
The sebaceous follicles are generally located on the face, but also on the shoulders, neck, back and upper chest.
They are clearly distinguishable from downy and terminal follicles, where the sebaceous glands are less developed.
To put it simply, it is the hair-to-gland ratio that distinguishes between these various types of pilosebaceous follicles.
Seborrhea
Sebum is a fatty substance produced by the sebaceous glands. It is intended to protect the skin and provide flexibility. Under normal conditions, the glands secrete just enough to keep the skin supple.
After secretion, the sebum passes from the sebaceous glands to the infundibulum, where it undergoes some changes before migrating to the skin surface via the pilosebaceous orifice: this is the excretion process.
But, in acne, this excretion process does not take place normally. The pilar canal used for the migration of sebum becomes blocked, which leads to an accumulation of sebum and the appearance of elementary lesions: microcomedones, comedones and microcysts.
Treating these lesions in time allows the dysfunction to be corrected and the sebum secretion and excretion processes to be set in motion.
In the event that these lesions are left untreated, they may progress to other more advanced lesions: the papules and pustules, the appearance of which is characteristic of inflammatory acne.
Characteristics of inflammatory acne
Thus, inflammatory acne is the result of inflammation of pilosebaceous follicles.
Indeed, sebum contains fatty acids that bacteria of the species Propionibacterium acnes – bacteria involved in inflammation – feed on to grow.
This inflammation is therefore a response of the body to the proliferation of bacteria. Thus, there is the appearance of papules that may develop into pustules.
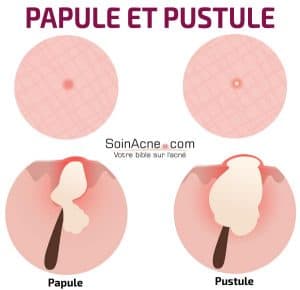
Papules
They usually arise from comedones, but can also appear spontaneously. Papules are firm elevations with a red coloration. They vary in size from 1 to 5 mm and can sometimes be painful.
Papules are an expression of inflammation of the sebaceous gland in which Propionibacterium acnes is involved. However, here the infection is always superficial. When no treatment is followed, they can lead to a more advanced stage: pustules.
Pustules
These are papules with a purulent yellow colored fluid on their apical part. They are the result of the development of many microbes on the same site.
They are slightly larger than papules and are frankly inflammatory. They can also develop into nodules, which are characteristic of severe acne.
Treatments for inflammatory acne
Based on the manifestations of inflammatory acne, several types of treatments have been developed. These treatments act in different ways. Indeed, some are designed to reduce lesions, while others directly attack Propionibacterium acnes to counteract the inflammation.
Thus, many treatments can be found in various forms. They are generally classified in two ways: the topical (local) treatments and the oral treatments.
Local treatments
Several topical agents can be used to treat inflammatory acne.
These include benzoyl peroxide, adapalene, and azaleic acid.
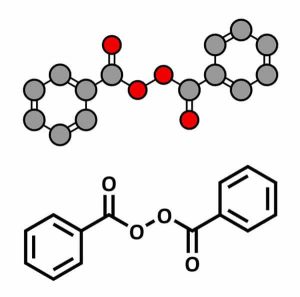
Benzoyl peroxide
When faced with inflammatory acne problems, the first treatment that can really provide relief is the application, once or twice a day, of benzoyl peroxide at 5% (Cutacnyl®, Papclair®…).
Indeed, benzoyl peroxide has anti-inflammatory activity and effectively fights bacteria. The latter cannot develop resistance, because the molecule acts through non-specific oxidation.
These characteristics of benzoyl peroxide mean that it can be effective against papules and pustules. In cases where the body can tolerate it, it is also possible to use a 10% peroxide preparation (Pannogel 10®, Eclaran10® Panoxyl®…). In the other direction, if the patient experiences irritation, it is possible to prescribe a 2.5% preparation (Cutacnyl®…)
Adapalene
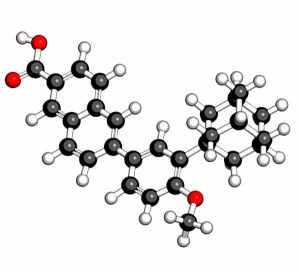
There may be cases where the body does not tolerate benzoyl peroxide at all. In these cases, there are other treatments such as adapalene at 0.1% (Adapalene TEVA®, Differine®…).
It is a topical retinoid possessing anti-inflammatory activity and thus helps to combat papules, pustules, and other elemental lesions (comedones and microcysts).
A topical antibiotic – such as clindamycin 1% (Zindacline®, Clindafluid®…) or erythromycin 4% (Eryacne®, Erythrogel®…) – can also be combined with adapalene or another topical retinoid such as tretinoin 0.025% (Erylik®).
One of the problems with topical retinoids is that they can have side effects. One of the most common is irritation.
To counter this risk, it is therefore advisable to use a non-comedogenic moisturizer during treatment.
Also note that pregnant women should not use retinoids, even if they are topical.
Azelaic acid
Another effective local treatment for inflammatory acne is azelaic acid.
It can be found, among others, in the form of a 15% gel (Finacea®) or a 20% cream (Skinoren®). This molecule has anti-inflammatory and keratolytic activity.
Oral treatments
With regard to general oral treatments, we can cite the use of antibiotics or, possibly, oral isotretinoin.
Antibiotics
Antibiotics applying are mostly from the cyclin family.
In some countries, these antibiotics may contain doxycycline (Doxycycline arrow®, Doxygram®, Tolexine® Gé…), or minocycline (Mynocine®, Minocycline Bayer®, Logryx®…).
However, given the rare but serious adverse effects, it is strongly recommended that not use minocycline as a first-line treatment. It should only be used in cases where other cyclins have failed acne and when oral isotretinoin cannot be used.
With regard to doxycycline, one of its side effects may be phototoxicity.
In specific situations, oral erythromycin (Abboticin®, Erythrogram® Gé…) can also be used, but in combination with local treatments: in fact, this is the recommended combination for oral antibiotics.
Thus, benzoyl peroxide or a topical retinoid can be chosen. The latter two can even be mixed under the recommendation of a professional. It should be noted that it is essential to consult a professional before combining treatments.
Isotretinoin
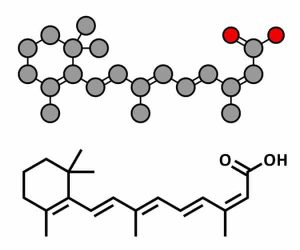
Another valid treatment for inflammatory acne is oral isotretinoin. It can be found in capsule form: Contracné® Gé, Curacné® Gé, Procuta® Gé…
If all previous treatments fail, this one may provide satisfaction. However, this molecule has many risks. Among these, we can mention the teratogenic risk.
It is therefore counter-indicated to pregnant women and women wishing to use it must combine its use with a contraceptive and do their pregnancy test regularly to be sure not to get pregnant during the treatment.
It is mandatory to consult a dermatologist before choosing this treatment: prescribing isotretinoin is strictly reserved for dermatologists (neither general practitioners nor other specialists are allowed to prescribe it).
Note, moreover, that it is strongly contraindicated to combine isotretinoin with an antibiotic (cyclin), as this exposes a risk of intracranial hypertension.