Page Content
This inflammatory dermatosis of the pilosebaceous follicle exists in several forms. These are distinguished by the processes inducing their development.
Retentional acne is one of the many forms of acne that exist.
It could simply be defined as an excessive accumulation of sebum in the pilosebaceous follicles. This is the consequence of hyperseborrhea and keratinization.
Hyperseborrhea
Hyperseborrhea refers to an excessive secretion of sebum. This secretion occurs mainly in areas such as the face, the central part of the back or the lower chest…
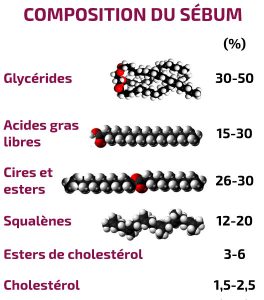
Sebum is an oily film whose role is to protect the skin against external aggressions and dryness. At a normal level, it gives the skin a good suppleness.
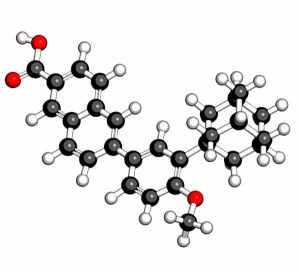
The maintenance and triggering of sebum is ensured by dihydrotestosterone.
This molecule is produced in the sebaceous glands from testosterone, under the action of 5α-reductase type 1.
When sebum is secreted by the sebaceous glands, the pilar canal must normally allow the secreted sebum to flow out to cover the skin, where it normally plays its protective role.
There are two concepts to be observed during the development of sebum: secretion and excretion.
The secretion refers to the actual elaboration of sebum; in other words, the flow of elaborated sebum passing through the excretory duct of the sebaceous gland to the infundibulum.
The excretion, on the other hand, refers to the amount of sebum flowing out of the pilosebaceous orifice after undergoing the changes in the infundibulum.
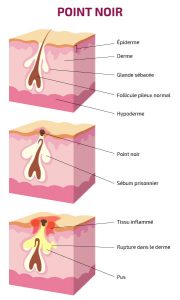
However, when acne occurs, the pilosebaceous canal becomes blocked, which causes an accumulation of elaborated sebum and the clogging of the canal by the accumulated sebum.
As a result, there is the appearance of two types of lesions: open comedones and microcysts.
Open comedones
This fluid is actually a mixture of keratinocytes – a type of cell that forms the lining of the hair shaft – and sebum. The black color of blackheads is explained by an oxidation of these keratinocytes.
This oxidation provides favorable conditions for the development of Propionibacterium acnes, the bacteria responsible for acne and likely to cause it to develop into its inflammatory form.
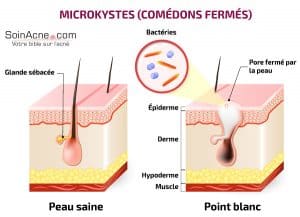
Microcysts
Microcysts (also known as closed comedones) are small white balls found under the skin. They can appear in various places on the body, but are particularly common on the hairline, temples and under the chin.
They are the result of an obstruction, by cells of the epidermis, of the orifice of the pilary canal of a pilosebaceous follicle.
When the sebaceous glands continue to secrete keratin and sebum, the skin eventually bulges and a pale area appears in the middle.
These pale areas appear as white balls because of the liquid they contain.
In addition, note that there is a particular form of microcysts called grains of milium. It is mainly found on the eyelids: they are actually superficial microcysts of very small size.
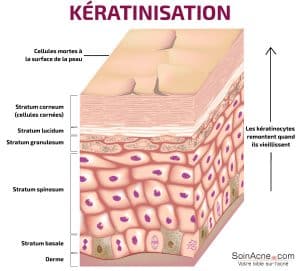
Keratinization process
Keratinization refers to the accumulation of keratin in epidermal cells.
Indeed, the establishment of comedones is related to a dysfunction of the keratinization process. This dysfunction results in hyperproliferation of keratinocytes in the follicular canal, hyperkeratosis and retention due to increased adhesion of horny cells.
Various factors are involved in the mechanisms of this increased proliferation and adhesion of keratinocytes.
Thus, we can note an anomaly in the control of androgens. Indeed, in the lower part of the infundibulum, there is an abundant quantity of 5 α-reductase compared to the rest of the epidermis. This is explained by an increase in androgen activity.
This excessive activity leads to abundant formation of androgen metabolites in keratinocytes, which interferes with their differentiation.
Disorders of keratinocyte differentiation would also be favored by the increase, in the infundibular canal, of the proportion of squalene and wax compared to that of linoleic acid.
Indeed, when squalene oxide and fatty acid levels are compared in acneic and control subjects, it is noted that these levels are higher in acneic subjects.
On the other hand, compared to the overlying surface of the epidermis, there is a deficiency of linoleic acid in the comedones. Furthermore, during the inflammatory reaction of the follicle, bacteria of the species Propionibacterium acnes stimulate the production of interleukin 1 by keratinocytes.
This production increases in the infundibulum and causes excessive cornification and scaling of the infundibulum.
The action of interleukin 1 could be through two mechanisms, direct and indirect:
- The direct mechanism would stimulate other growth factors or involve interleukin-1 receptors.
- In the indirect mechanism, interleukin 1 would mediate the rate of sebaceous excretion and the degree of acne severity.
Treatment of retentional acne

Retentional lesions of open (blackheads) and closed (microcysts, or whiteheads) comedones on the forehead of a teenager ©thamkc/123RF
For retentional acne in particular, the most suitable treatment is a topical treatment. The latter can sometimes also be combined with general treatments: the goal being to stop the development of bacteria.
Note, however, that although they have proven effectiveness, these medications can cause photosensitization.
In order to treat retentional acne, it is possible to distinguish between topical retinoids, benzoyl peroxide and azelaic acid.
Topical retinoids
In terms of retinoids, we can distinguish three molecules: the tretinoin, the isotretinoin and the adapalene.
These molecules work primarily on microcysts and comedones.
Tretinoin
Still called all-trans retinoic acid, tretinoin is the oldest of the retinoids. It can be found as a gel, cream (Retin-A®, Effederm®…), or as a 0.025%, 0.05% and 0.1% solution.
It can be used alone or in combination with erythromycin. Most of the time, it causes irritation at the beginning of treatment, which diminishes when combined with erythromycin.
Tretinoin can also be the cause of certain irritant reactions. In this case, a reduction in its quantity, concentration or rate of application may help.
Isotretinoin
Isotretinoin (Roaccutane®, Curacne®…) is a isomer of tretinoin. Thus, there is no fundamental difference between the two molecules.
For the treatment of retentional acne, isotretinoin is better tolerated.
It can be found, among others, as a 0.05% gel, combined with erythromycin 2% or not.
Adapalene
Adapalene is a naphthoic acid derivative that acts similarly to retinoids. It has anti-inflammatory activity which makes it effective against inflammatory acne as well.
The first signs of improvement can be seen after one to four weeks of treatment with adapalene. This topical retinoid is available as a 0.1% cream and gel (Differine®).
Compared to tretinoin 0.05% cream, adapalene is better tolerated (because it is less irritating) for the treatment of retentional acne.
Note, moreover, that local retinoids have risks of teratogenesis (hence the special conditions for prescribing in women of childbearing age).
It is often advised to avoid using tretinoin preparations during the first 3 months of pregnancy, although – according to the teratogenic agents referral center – the data for pregnant women exposed dermally are rather reassuring.
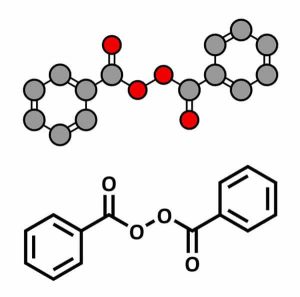
Benzoyl peroxide
At the beginning of the treatment, it can irritate the face. In cases where sufferers have dry skin, an application in the evening with a low concentration can reduce this sensation, especially in sunny periods.
In addition, the application of a moisturizing or softening cream can reduce the side effects.
Benzoyl peroxide (Cutacnyl®, Brevoxyl®…) is available as a gel, lotion, cream or pad; and in concentrations of 10%, 5% and 2.5%.
In addition, it should be noted that the combined use of benzoyl peroxide and adapalene or benzoyl peroxide and clindamycin (Duac®) improves therapeutic adherence.
Azelaic acid
In the fight against acne, it can either replace retinoids and antibiotics or be used in combination with them.
Some of its commercial forms are Skinoren® and Finacea®.
Final words
It should also be noted that there are many other treatments and medications that can be used in place of the above examples.
In addition, it is important to remember that there is a lot of information involved in determining the appropriate treatment regimen for acne.
For example, it is possible to take into account the age of the patient, the extent of the acne, the duration of the evolution…